M.B.B.S Final Practical Examination Short Case - 1701006038
D. Gaurav Singh
1701006038
DE-IDENTIFIED CONSENT FORM :
A 46 year old male came to casuality with chief complaints of
-burning micturition since 10days
-vomiting since 2days (3-4 episodes)
-giddiness and deviation of mouth since 1day
History of presenting illness:
Patient was apparently asymptomatic 10years back, he complained of polyuria for which he was diagnosed with Type 2 diabetes mellitus he was started on oral anti diabetic medication, 3years back oral medication were converted to insulin.
20days back he developed vomiting containing food particles, non bilious,non foul smelling(3-4 episodes),later he complained of giddiness and deviation of mouth for which he was brought to our hospital
No history of fever/cough/cold
No significant history of UTIs
Past history:
10years back patient complained of polyuria for which he was diagnosed with Type 2 Diabetes Mellitus, he was started on oral hypoglycemic agents(OHA) 10years back
3years back OHAs were converted into Insulin
3years back he underwent cataract surgery
1year back he had injury to his right leg, which gradually progressed to non healing ulcer extending upto below knee and ended with undergoing below knee amputation due to developement of wet gangrene.
Delayed wound healing was present- it took 2months to heal
Not a known case of Hypertension, Epilepsy,Tuberculosis, Thyroid, Asthama.
Not on any medication
No history of blood transfusion
Personal history:
Diet - Mixed
Appetite- normal
Sleep- Adequate
Bowel and bladder- Regular
Micturition- burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Regular consumption of alcohol, about 90mL whiskey consumed almost daily.Also 1 month on & off consumption pattern previously present
Family history:
Not significant
Vitals during Admission:
BP: 110/80 mmHg
HR: 98 bpm
RR: 18 cpm
TEMP: 99F
SpO2: 98% on RA
General Examination:
Pallor present
No- icterus,cyanosis,clubbing,koilonychia, lymphadenopathy
No dehydration
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)Normal
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
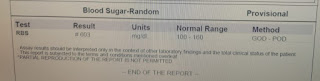
Investigations:
Culture report: Klebsiella Pneumonia positive
Pus cells
Provisional Diagnosis:
pyelonephiritis with h/o of Type 2 Diabetes mellitus since 10years and amputation below knee