57/M with ALTERED SENSORIUM SECONDARY TO HYPOGLYCEMIA
A 56 year old male patient who is a resident of koilagudem (nalgonda district)who is a daily wage labourer by occupation brought to the casualty in unresponsive state at 1:30 Am .patient was found drowsy from 1 pm on 25/04/2023 And suddenly developed seizure like activity associated with slurring of speech,uprolling of eyeballs,stiffness of all four limbs,
Associated with involuntary defecation and micturition and found unresponsive.
No h/o fever ,cough.
No h/o neck stiffness and projectile vomitings.
No h/o generalised weakness ,tingling,numbness.
No h/o head trauma.
Patient was apparently asymptomatic 6 months back then he developed multipleSwellings Over the Cheek, Forearm, legs with dischargingPus with no pain. for which he went to an RMP and he prescribed Antibiotics but it resolves on for some days and then reappears in 10-15days. He also developed swelling on the nose 6 months back the RMP Removed the pus ,After somedays it healed but the nose became a saddle nose.
1 month back He developed Edema of legs which was insidious in onset and gradually progressive in nature which is progressed from ankle to knees which is of pitting type. for which they went to hospital and was diagnosed with DM2 and .on glimiperide 1mg and metfromin 500mg.
PAST HISTORY:
No history of similar complaints in the past.
Known case of Diabetes type 2 since 1 month.on glimiperide 1mg and metfromin 500mg.
known case of asthma since 30 years.
Not a known case of Diabetes,HTN,Epilepsy,CAD,TB.
DAILY ROUTINE:Patient is a daily wage labourer by occupation he stopped his occupation 6to7 years ago because he vision becoming cloudy and he is getting old
DAILY ROUTINE OF THE PATIENT BEFORE DIABETES
He daily wakes at 5AM and he does his daily activities and fresh up ,takes bath and drinks decoction 7am and then at 10 am he take his breakfast which contains rice with curry and after taking his breakfast he chit chat with neighbors and lie down for sometime and then In the afternoon at 1pm or 2pm he takes his lunch which consists of rice as well as some vegetable curry and after that he sleeps for some time watch TV and drinks decoction at 5pm and at 8pm he takes his dinner which consists of rice and a vegetable curry and night he sleeps at 10 pm .he has the habit of drinking decoction in the night like tow times at 12or1am and at3 or 4 am.
DAILY ROUTINE OF THE PATIENT AFTER BEING DIAGNOSED WITH DIABETES .
PATIENT REDUCED TAKING DECOCTION TOO FREQUENTLY AND STARTED TAKING ONLY IN THE MORNING AT 7AM AND HIS MEALS(RICE WITH CURRY) WERE REPLACED BY GADAKA(PORRIDGE)AND JONNA ROTTE (JOWAR ROTI).3 TIMES A DAY.
FAMILY HISTORY:
No similar complaints in the family.
PERSONAL HISTORY:
DIET : MIXED
APPETITE: ADEQUATE
SLEEP:NORMAL
BOWEL AND BLADDER :REGULAR
ADDICTIONS: NO ADDICTIONS.
TREATMENT HISTORY:
DELPHILIN AND DACADRAN SINCE 30 YEARS (SOS)
GENERAL EXAMINATION:
Patient is unresponsive.
Pupils dilated sluggishly reactive.
Poorly built and poorly nourished.
Vitals: Pulse rate during admission 52 bpm on atropine 98bpm.
Respiratory rate:32cpm.
Spo2 :98%@RA.
Bp:120/90MMHG
Temp:afebrile.
SYSTEMIC EXAMINATION:
CVS:S1,S2 HEARD,NO MURMURS.
RS:BAE+,NVBS.
P/A: SOFT ,NON TENDER.
CNS: Patient is unresponsive at first.
HMF:INTACT
MOTOR EXAMINATION
TONE: rt lt
UL: N. N
LL:N N
REFLEXES:
B:2+ 2+
T:2+ 2+
S:2+ 2+
K:2+ 2+
A2+ 2+
P:2+ 2+
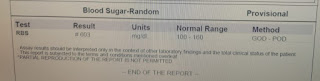
INVESTIGATIONS AND CLINICAL IMAGES:
26/04/23
PROVISIONAL DIAGNOSIS:
ALTERED SENSORIUM SECONDARY TO ?HYPOGLYCEMIA.
Treatment:
1IVF NS @@ 50ml/hr.
2.Inj:25%DEXTROSE INFUSION @10ml/hr
Increase/decrease according to GRBS.
3.INJ:PIPTAZ 4.5 g/Iv/TID
4.Inj.CLINDAMYCIN TID
5.TAB.DOLO 650 mg/po/(sos)
................FOLLOW UP....................
27/04/2023
S:
No fever spikes
Stools passed (4episodes of loose stools)
His swellings on the forearm was not subsided and pus is sent for c/s
O:
Patient is conscious,coherent,cooperative
Temp:99.6°F
BP:100/70mmhg.
PR:80bpm.
RR:20cpm.
CVS:S1,S2HEARD ,NO MURMURS.
RS:BAE+,NVBS.
GRBS:437mg/dl.
A:ALTERED SENSORIUM RESOLVED.
RECURRENT HYPOGLYCEMIA 2°TO ? LEFT UPPER LOBE ABSCESS.
WITH ANEMIA(NORMOCHROMIC NORMOCYTIC).
WITH HYPOKALEMIA 2°TO GI LOSSES, WITH DM2 SINCE 1 MONTH
P:
IVF-NS@75ml/hr.
INJ:25% DEXTROSE INFUSION @45ml/hr.
INJ:PIPTAZ 4.5 g /iv/TID.
INJ:CLINDAMYCIN 600mg/iv/TID.
Tab.DOLO 650mg/po/sos.
Tab.SPOROLAC PO/TID
QUESTIONS IN THE ROUNDS....
1.GOLD STANDARD TEST FOR WEGENERS
https://pubmed.ncbi.nlm.nih.gov/14968341/
2.WHY IS HYPOGLYCEMIA IN THIS PATIENT??
3.DANGER AREA OF FACE??
4.WHY DOES SEPSIS CAUSE HYPOGLYCEMIA???
5.HOW IS CBNAAT DONE??
28/04/2023
S:
No fever spikes
Stools passed (2episodes of stools)
O:
Patient is conscious,coherent,cooperative
Temp:Afebrile
BP:110/60mmhg.
PR:76bpm.
RR:19cpm.
CVS:S1,S2HEARD ,NO MURMURS.
RS:BAE+,NVBS.
P/A:SOFT,NONTENDER.
GRBS:129mg/dl.@9AM
A:ALTERED SENSORIUM( RESOLVED) 2°TO HYPOGLYCEMIA(RESOLVED) WITH LEFT UPPER LOBE ABSCESS WITH
WITH ANEMIA(NORMOCHROMIC NORMOCYTIC).
WITH HYPOKALEMIA 2°TO GI LOSSES, WITH DM2 SINCE 1 MONTH
?WEGENERS GRANULOMATOSIS
?CHURG STRAUSS
HYPOGLYCEMIA RESOLVED
P:
IVF-NS@75ml/hr.
INJ:PIPTAZ 4.5 g /iv/TID.
INJ:CLINDAMYCIN 600mg/iv/TID.
Tab.SPOROLAC PO/TID
SYP:POTCHLOR 15ml/PO/TID
SYP.ARISTOZYME 15ml/PO/TID.
PLANNING FOR SPLIT SKIN SMEAR.
☆SPLIT SKIN BIOPSY WAS NOT DONE ON 28/04/2023 BECAUSE THE PATIENT BECAME HYPOTENSIVE DURING THAT TIME.
☆WE REFERRED THE PATEINT TO ENT THEY DID DNE
▪︎This is the YouTube video showing is DNE☝
ALTERED SENSORIUM( RESOLVED) 2°TO HYPOGLYCEMIA WITH LEFT LUNG UPPER LOBE ABSCESS WITH CUTANEOUS ABSCESS (MRSA) ?WEGENERS GRANULOMATOSIS
?CHURG STRAUSS
WITH ANEMIA(NORMOCHROMIC NORMOCYTIC).
WITH HYPOKALEMIA 2°TO GI LOSSES(RESOLVED), WITH DM2 SINCE 1 MONTH.
Bronchial asthma since 30 years
56 year old brought to the casualty in unresponsive state at 1:30 Am .patient was found drowsy from 1 pm on 25/04/2023 And suddenly developed seizure like activity.
Patient was apparently asymptomatic 6 months back then he developed multiple swellings over the Cheek, Forearm, legs with discharging pus with no pain for which he went to an RMP and he prescribed Antibiotics but it resolved for some days and then reappeared in 10-15 days. He also developed swelling on the nose 6 months back and the RMP removed the pus.,After somedays it healed but the nose became a saddle nose.
1 month back He developed Edema of legs which was insidious in onset and gradually progressive in nature which is progressed from ankle to knees which is of pitting type. for which they went to hospital and was diagnosed with DM2 and .on glimiperide 1mg and metfromin 500mg.
Past history :
Bronchial asthma since 30 years on deriphylline and Decadron SOS
Course in hospital :
Patient was investigated further and found to have left upper lobe lung abscess other than his cutaneous abscesses and also investigated for his saddle nose with no mucosal abnormality on nasal endoscopy. Biopsies from skin were sent and report is awaited. He's being discharged and asked to follow with the report of the biopsy.

















































.jpeg)










